Are You Childhood Cancer Aware?
Sunday September 3, 2017 | Abby White, WE C Hope CEO
Abby White, WE C Hope co-founder and volunteer CEO, shares her experience of living with the consequences of bilateral retinoblastoma, and her very personal journey to the organization’s birth.
Childhood Cancer Awareness Matters!
Why is it important? Why should we be concerned when childhood cancer accounts for only 1-3% of all cancer cases?
There is a general belief that childhood cancer has a low impact on society, and on childhood deaths, because it is rare. This is totally untrue.
With insights from parents and survivors, we explore the realities of childhood cancer.
September shines gold for childhood cancer.
The Biggest Child Killer
Childhood cancer is uncommon, but it is the leading cause of death by disease in children in developed countries – more than asthma, diabetes, cystic fibrosis and AIDS combined. Cancer is also the second most common cause of death by disease, and the leading cause of non-communicable disease, among children aged 1 to 15 in the developing world.
It is torture to remember how I photoshoped a black pupil on the whiteness In Anali’s eye. Oh dear God how many more years of life she could have had, if we had only known.
Parent, Brazil.
Most childhood cancer is curable, but delayed diagnosis significantly reduces a child’s chance of survival. In developing countries, 7-8 out of 10 children will die – mostly due to late presentation at the hospital and lack of well-equipped, specialised units. In developed countries, 1-2 in 10 children will die, due to delayed diagnosis, or diagnosis that remains difficult to treat. A few cancers, such as retinoblastoma and osteosarcoma, record higher rates of preventable death due to excessive effort to save the child’s affected eye or limb.
We were absolutely floored when the cancer came back after enucleation (unilateral Rb). We did lots of chemo and the transplant, but it didn’t work.
When everyone said there was no hope of cure, we were damaged again because no one knew what to do next, what therapy to limit the symptoms and give good quality of life and time. Every new event was a mini earthquake and we could find little info online to help guide us. I know our situation is rare, but there needs to be more work so families like ours don’t suffer in that void when we are already devastated.
Parent, USA.
The International Society of Paediatric Oncology recognizes that more than 90,000 children worldwide die needlessly every year. 90% of these preventable deaths occur in developing countries.
Our local clinic advised us to go to the main hospital to see an eye surgeon, but we had no way to get there and pay the bill. We didn’t know how much it would be, but we knew we couldn’t pay.
By the time we came to the hospital, the cancer was big and we have been told nothing can be done now.
We were just told to go to the eye hospital, not that our child had cancer or could die. If you’re told to see an eye doctor, you don’t think the thing can kill.
Parent, India.
* * *
We were sent to five different hospitals before we got to the right place that could treat our daughter. The local clinic referred us to a church mission clinic, who sent us to the district hospital, where we were passed to the regional hospital. They said we must go to the city but by that time it was 3 months later and we had no money left. We really struggled.
There needs to be a plan to get children quickly to where they need to be for the correct treatment. That would save a lot of time and money and give the child a better chance of being cured.
Parent, Tanzania.
Childhood Cancer is Different from Adult Cancer
Most adult cancers are strongly linked to lifestyle choices or environmental risk factors. Their development can be prevented, or risk reduced by living well and limiting exposure to cancer-causing toxins such as tobacco, alcohol and ultraviolet light.
Cancers affecting children are often caused by DNA changes in cells that occur very early in life, while the body is rapidly developing. Sometimes these changes can cause cancer to form even before birth, as in the case of retinoblastoma. Unless the cancer is caused by an inherited genetic mutation, these DNA changes cannot be anticipated and they cannot be prevented.
When my second child was born I thought I was ready for anything because I had done this before. I was used to diapers and sleepless nights and I loved holding my son in my arms.
My daughter was born a week before her due date and was a whopping 9 lbs. But she would cry whenever we had the lights on or the blinds open. This behavior continued for MONTHS. I wondered why I had a baby who wanted to live in a dungeon. My OB and pediatrician said “she has been living in a dark womb for 9 months and just hasn’t adjusted yet – give her more time.”
I gave it time until I asked her pediatrician to take a good look at her well baby check up. She was diagnosed with bilateral retinoblastoma at four-months-old. I’m grateful to her doctors for saving her life, but I will always wish I had borne the knowledge of retinoblastoma before my daughter was born, rather than four months after.
Parent, USA.
* * *
Why is retcam only used to examine preemie babies at birth? If it’s in the baby unit to check for ROP, why so impossible to extend access to all newborns?
My son had unilateral Rb, so advanced at diagnosis (10 months) that it was most likely there at birth. He was in the NICU for jaundice. I saw a retcam in the hallway, but not for my son! That simple exam could have saved his eye and his sight, and spared him 6 gruelling months of chemo (that included his first birthday and Christmas).
Parent, USA.
Various studies show that 50-80% of children have advanced disease at diagnosis, compared with 30% of adults. This very clearly demonstrates poor awareness of childhood cancer among parents and primary health workers caring for children and teenagers.
Our daughter never had white eye show in photos. She only had an increasingly pronounced squint. If she hadn’t had an eye exam when we changed GPs, she might not have been diagnosed until very late.
Despite not having white eye, her cancer was still E and her eye was removed a week later.
White eye awareness is promoted. Squint less so. Most doctors say kids will grow out of squint and that is true, but we shouldn’t risk kids by playing down the possibility the squint is something more sinister.
Parent, UK.
* * *
Primary doctors (GPs and paediatricians) need to be much more willing to listen to a parent’s concerns, and follow through on the parent’s informed request.
My child had different coloured irises, squint, then intermittent white eye photos, progressing to every photo and then seen with my naked eye. Different doctors repeatedly fobbed us off with “it’s normal for her age” or “it’s just the camera”. There is often talk of parents being in denial about childhood cancer. What about the endemic denial among doctors?
Parent, UK.
* * *
The average age of children at diagnosis is 6 years, compared with 67 years among adults. 95% of children with retinoblastoma are under 3 years old at diagnosis. So children have many more years of productive life ahead of them. Therefore, death and poor quality of life due to effects of childhood cancer and its treatment have significantly more societal impact than does cancer in adulthood.
Childhood Cancer Has Lifelong Consequences
The average length of cancer treatment in children is longer than for adults, as are recorded hospital admissions. Although statistics vary, particularly in relation to cancer type, the difference remains significant. Childhood cancer treatment can last more than 3 years – that’s over 1,000 days of learning, growing and innocence disrupted or lost forever, with potentially major impacts on the child throughout life.
Can Post Traumatic Stress happen years after Rb? Our whole family went through four years of hell with our daughter’s treatment. We were walking around in a daze for another two years,
Nearly five years later, my daughter is healthy, but she is not happy. She’s often moody and withdrawn, and cries easily, especially about anything medical.
I feel my entire family, to some degree has PTSD. Psychology support would have been very helpful.
Parent, USA.
* * *
As children’s bodies and minds are developing during cancer treatment, side effects of therapy can have life-long impact on physical and emotional development. The American Cancer Society reports that more than 60% of children who survive cancer suffer late-effects such as infertility, heart failure and second primary cancers. Long term side effects are much less prevalent in adults, whose bodies are fully developed at the time of diagnosis and treatment.
At the beginning everyone goes through it with you, and then after time, when things calm down, you are left to your own devices by most people, except a few immediate family and friends. People do not know what you go through every day, and I often get ‘he’s ok now’ or ‘he can see now’, but he has been left scarred and partially sighted and experiences difficulties everyday. I think it is then you need support still.
Parent, UK
* * *
This is a lifelong issue for all involved. Not treat, cure, good luck and see you later. Then there’s years later…RB didn’t take my child’s life. But now what? Where do we go from here? The teen years above and beyond are quite unsupported and left to one’s own devices.
Parent, Australia.
* * *
I had unilateral Rb. Genetic testing ensured my son’s early diagnosis and both his eyes were saved. I am so thankful, and firmly believe testing must be integral to patient care.
However, I am distressed by lack of investment in research to improve long-term outlook for survivors.
My vulnerability was exposed by recent removal of a benign tumor. Rb survivors are a close-knit global community thanks to the internet. We lose friends to second cancers every month; each loss mutilates our collective heart.
Surely science is at a point where prevention can become a reality? When will you recognize our life-long agony and help extend to us the same hope you have given to our children?
Survivor and Parent, USA.
* * *
As a survivor, things that frustrate me most are lack of Rb specific follow up care and lack of awareness among even general ophthalmologists, let alone GPs about my life-long risks and treatment late effects.
I had cancer – I shouldn’t have to ask or struggle to find out what I need in terms of health care follow up. I know long term follow up and late effects clinics are now commonplace for kids recently treated, but we “old timers” should also be plugged into that care. We shouldn’t have to beg to be seen!
Survivor, UK.
* * *
I had Rb as a baby and have the RB1 mutation. I know my risks, but it seems I am the only one who does, other than my original doctors, who are retired.
I have no follow-up, for ophth or ongology. My GP doesn’t understand Rb or my mutation and thinks I am neurotic – she thinks I need to see a psychiatrist.
I am so worried that one day the other shoe will drop and my diagnosis will come too late because no one is following me or paying attention to my risk.
Survivor, Australia.
Childhood Cancer Impacts on the Whole Family
Adult cancer care is generally accessible at most large hospitals. However, childhood cancer care is provided at specialist units that are widely dispersed, and often not located close to the family home. This can mean separation of the family and disruption of family life for months, or even years during treatment, at a time when the family most needs to be together in familiar, safe and nurturing surroundings.
The physical effects of retinoblastoma can sometimes feel so much more manageable then the psychological effects.
Parent, USA.
* * *
Sometimes I just need a friend to put her arms around me and hold me, especially when I am in the hospital with my daughter, so far from home.
Parent, Canada.
* * *
I truly appreciated people who asked ‘how are you’, listened to the standard ‘ok’ reply, and then asked again ‘yes, but how are you really’? I knew then that they were totally there with me, actively listening and empathising.
Parent, USA.
* * *
Our daughter’s diagnosing doctor told us we must go to an Rb specialist, and the specialist said chemo must begin right away. Our insurer refused to cover treatment there, insisting we go to their preferred in-network provider, which is a major ped-onc center but has no expertise in treating Rb.
I believe if there were some way to clearly identify a center’s Rb care credentials, insurers would be more co-operative at a time when prompt action is critical.
Parent, USA.
* * *
We need a way in which absent partners can be more involved in the treatment / follow up process.
I could only attend the first crisis EUA and surgery. My job carries the insurance and I’d already taken time off to help care for my elderly father. I feel terrible that my wife carried most of the stress alone – I am the dad, I am supposed to protect my family.
I wish we’d had a teleconference option so I could be at the consultations and support my wife in them.
Parent, USA.
* * *
I think it needs to be made clearer to families that St Jude can’t accept patients if they begin treatment elsewhere. We were suggested to go there, but we live near the Pacific Canadian border and it seemed so far when we needed our family close by.
We decided we would go there if the first option closer to home didn’t work, but when that time came, we were dismayed to find we couldn’t go there for care because of our earlier choice. If we’d been told this would be a problem, we’d have gone there first.
Parent, USA.
* * *
During our chemotherapy, three children on our ward left because the family lost hope. The bills, lack of privacy, support and information all suffocated them.
Maybe the children could have been cured, maybe not, but they should have had an equal chance. A year later we brought toys to the ward that our son grew out of, and one of the children was back there, in such terrible pain and with a huge mass. The memory breaks my heart. He could so easily have been my son, but for my husband’s good job.
Parent, Nigeria.
* * *
What we found hardest was how slow the wheels turned at our hospital. We had to wait at the hospital a whole day to confirm a bed for treatment. We had to take our child’s blood samples to different labs and the reports took forever to come back.
When he was sick from chemo in the middle of the night, there was no doctor available and the nurses wouldn’t act without the doctor’s direction. So those nights were very hard for us.
Inefficiency really sapped energy and we were constantly exhausted, body and mind.
Parent, Malaysia.
* * *
I wish I’d known the value of child life from the get-go. We thought as he was only 3 months, it couldn’t help. No child life person came to see us anyway.
By the time we met a wonderful child life specialist willing to work with us, the damage was done and it has taken a long time to even begin to undo some of that negative impact.
Child life should be a fully integrated part of the care package from the moment of pre-diagnosis EUA, not an optional extra or a last-resort solution.
Parent, USA.
* * *
75%+ of families caring for a child with cancer will experience financial hardship after diagnosis. In most families, at least one parent will reduce working hours or leave work completely to care for the sick child, often with the loss of employer-linked medical insurance. At the same time, they encounter higher costs medical bills (in many countries), increased travel to specialist hospitals and costs of living away from home.
I work for a large company that is full of nameless people. When my daughter was on chemo and my own leave was all used up, a group of people I didn’t know came to my office and told me they wanted to give me their vacation time so that I wouldn’t lose a pay check. My mouth dropped open! Sacrificing leave for a stranger is just about the greatest gift anyone has given me.
Parent, USA.
* * *
My husband works at an auto repair shop. At one point, his boss told him he was missing too much work, and might lose the job if he didn’t increase his hours. This was an awful time of uncertainty, because we have always approached our children’s cancer as a team, and we always attend the doctor consultations together. One of his co-workers realized the problem and suggested the remaining staff each take a little over-time to ensure my husband’s share of the work was done. The boss was happy with that – so long as no one expected to be paid for the overtime. My husband kept his job, and our family stayed afloat because of those people.
Parent, USA.
The US National Institute of Health estimates that more than 25% of total family income is consumed by medical costs and related expenses during a child’s cancer care, even when the family is fully insured. The family of an inadequately insured child is likely to incur significant debt, and some have even lost their home in efforts to ensure their child receives treatment.
We would have appreciated financial support. It isn’t just the treatment itself that can be financially draining, but also the travelling and the living costs away from home. We didn’t feel we could ask for this kind of help, but would have gladly accepted it if people had offered.
Parent, USA.
* * *
When Sarah was rediagnosed with trilateral retinoblastoma, it took us by complete surprise. We gratefully accepted some financial help from our parents. They helped us with buying things such as clothing, food, and taking care of our older son’s basic financial needs. These things may seem small to some people, however, since we were far from home during her treatment, we appreciated any help we were given.
Parent, USA.
* * *
These challenges and threats are magnified significantly for families in developing countries, where there are no buffers provided by social security systems, scarce support organisations and few people with disposable income in the community who can offer assistance.
Even in countries with full insurance or a national health system, such as Canada and the UK, many families face extra financial burdens during their child’s illness.
Money worries heap great stress on the already overwhelmed family, and most require some form of financial assistance during treatment and beyond. In September 2016, CLIC Sargent reported that 76% of UK families experienced significantly increased stress and anxiety managing their finances after diagnosis.
It was hard accepting money from people, but at the time we really needed it or we wouldn’t have been able to stay in our home.
Parent, USA.
Know the Early Warning Signs of Cancer in Children!
The earlier cancer is diagnosed, the easier it is to treat. Often it requires less intense therapy and fewer invasive procedures that have lower cost physically, emotionally, socially and financially.
Awareness is key to achieving early diagnosis, saving lives and limiting the burden of cancer treatment on the child, family and wider society.
I threw away so many pictures, thinking there is a problem with the flash. I did not even know cancer can come in the eye. I think I am an educated man, but I did not know how to protect my son by this way. How did I not know this simple thing?
Parent, Poland.
Remember the SILUAN signs of childhood cancer:
Seek medical help early for persistent symptoms.
- Eye: white spot in the eye, new squint, new blindness, bulging eyeball.
- Lump in the abdomen, pelvis, head,neck, limbs, testes or glands.
- Unexplained prolonged fever for over 2 weeks, loss of weight, pallor, fatigue, easy bruising or bleeding.
- Aching bones, joints, back, and easy fractures.
- Neurological Signs: change or deterioration in walk, balance or speech, regression of milestones, headaches for more than a week with or without vomiting, enlarging head.
Compiled by the South African Children’s Cancer Study Group. Adopted by the International Society of Paediatric Oncology.
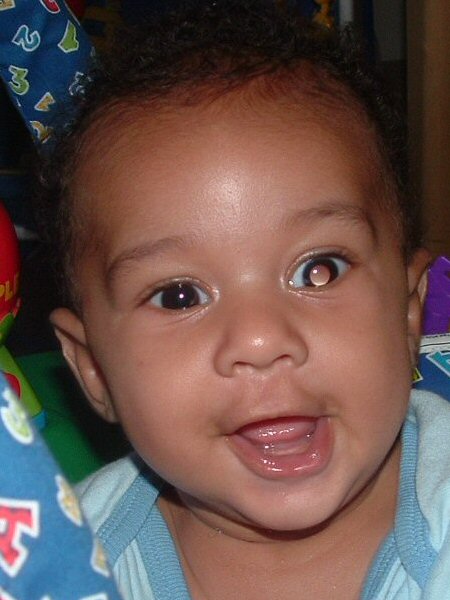
Leukocoria, a white glow in the pupil of the eye that may be a sign of retinoblastoma or another potentially blinding eye condition.
Join Us at One Rb World 2024 in Hawaii
Retinoblastoma awareness and early detection is a global challenge. There is no single solution to diagnose children early, but many opportunities exist to improve early diagnosis in all regions of the world.
National and global collaboration between retinoblastoma specialists, researchers, parents, survivors, and other advocates can dramatically improve care and cure for each child with eye cancer.
If you would like to join this global community sharing knowledge and experience, learning from one another, and exploring priority subjects together, we welcome you to the 7th One Rb World meeting, October 15-17 2024 in Honolulu, Hawaii. The meeting will be held just before the International Society of Paediatric Oncology World Congress which takes place 17-20 October, 2024 at the Honolulu Convention Centre.
One Rb World is community, conversation, and cooperation. An inclusive global collaboration for optimal lifelong care. Children are welcome too – One Rb World is proud to offer a full child life program for Rb patients, young survivors, siblings, and children of adult survivors!





Leave a Reply
Want to join the discussion?Feel free to contribute!