How Do We Achieve Early Diagnosis?
Updated Monday August 12, 2019 | Republished Saturday May 13, 2017 | Originally Published Saturday March 9, 2013
Early diagnosis of retinoblastoma is vital to save a child’s life and sight with minimally invasive therapies. But achieving early diagnosis is not simple nor easy. WE C Hope CEO, Abby White, explores various routes to awareness and diagnosis, and how they can impact patient care.
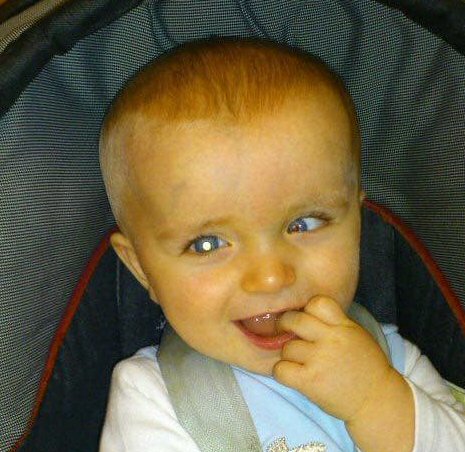
A baby has white pupil (leukocoria) in his right eye and squint (strabismus/crossed eyes) in his left eye – the two most common signs of retinoblastoma.
Retinoblastoma specialists agree that early diagnosis of eye cancer is a child’s best hope of survival, retaining some vision or their eye. In many parts of the world, early diagnosis is a child’s only hope of cure. Yet in developed countries, many children are diagnosed at a stage when removing their eye is the only treatment option for survival, and in developing countries, thousands of children die.
Early detection is one of the greatest challenges facing the retinoblastoma world. Most affected families have a harrowing story to tell of white pupil photos going unnoticed due to lack of awareness. They tell of doctors dismissing leukocoria and squint and other symptoms as “normal” or not listening to parental concerns and failing to refer to an ophthalmologist. Many describe being referred through multiple doctors and hospitals before a diagnosis was finally made. All these barriers waste precious time and often very limited resources.
So what is the answer? Many solutions have been proposed, including the use of complex retinal function and imaging technology, and non-invasive mandated screening of the red reflex. Or, simply providing parents information on signs or symptoms to be aware of and how to seek health advice. Her e we consider the potential and limitations of each of these approaches.
The Retina and Retinoblastoma
Before we explore the different approaches to retinoblastoma awareness for early detection, it is important to understand the structure of the retina.
The retina is not confined to the back of the eye, as is often described. The retina forms about 72% of the eye’s inner lining, from the optic nerve at the back to the ciliary body surrounding the iris (coloured ring) at the front. The junction of the retina and the ciliary body is called the ora serrata.
Only the posterior pole, encompassing the optic nerve and macula, is clearly visible on dilated eye exam. This posterior pole makes up about 2.1% of the retina and enables detailed vision. The remaining 97.9% is referred to as the peripheral or anterior retina.
Retinoblastoma forms when genetic mutations occur during normal cell division as the retina continues to grow from posterior pole outwards. Tumours at the posterior pole affect vision the most, even when they are very small. Tumours can arise anywhere on the retina, and the older the child is when they form, the further forward they will be.
Note the difference between “anterior tumour” and “anterior chamber”: “Anterior tumour” refers to cancer arising in the anterior retina. The anterior chamber forms part of the aqueous humor, in front of the iris. When retinoblastoma invades the anterior chamber, the child’s life is at risk as cancer can easily spread through blood vessels to the bone marrow.
Click on either of the images below to enlarge them.
Internal structure of the eye.
Structure of the retina, which forms about 72% of the eye’s inner lining.
Mandated Red Reflex Test at Birth
Cancer in infants can be seen with a simple red reflex test as tumours in this age group form in the easily visible posterior pole. However, most newborns with retinoblastoma are already identified as at risk, due to retinoblastoma in a blood relative. So while a simple awake red reflex test could be very valuable in detecting various eye conditions present at birth, if would detect only a small percentage of retinoblastoma in unsuspecting families.
Mandated Well Child Red Reflex Test
There is a general belief that regular eye exams, including red reflex tests, performed by primary care physicians will dramatically improve early detection of retinoblastoma. However, awake eye exams, even with dilating drops, enable clear examination only of the posterior pole. No published research has documented the proportion of retinoblastoma arising from the posterior pole, but anecdotally, less than 30% of tumours form in this area.
Small anterior tumours are usually only visible when the eye is examined under general anaesthesia. This is because the eye must be significantly manipulated to view these parts of the retina and this cannot be done on an awake child. Anterior tumours don’t cause consistent, obvious squint or white pupil in photographs or awake exams until cancer invades the posterior pole or central parts of the eye, by which time the tumours are usually large.
Mandated screening for retinoblastoma also relies on the primary doctor performing the red reflex test correctly. There is a high risk of cancer being missed on exam, either because tumours are located in the anterior retina, because the exam has not been done correctly, or because the child is unable to co-operate with the exam. A “clear” exam result could give a parent false reassurance, and stop or delay them from advocating appropriate care when they see signs the doctor is unable to observe.
Red reflex tests during well child exams are definitely important, but they are far from a panacea. Educating primary health workers to listen to parent and carer concerns, and refer promptly to an ophthalmologist, is likely to be far more effective in achieving early diagnosis.
We Are TLM explains why it’s important to ask for an eye exam when parents see squint, white eye glow or a painful red eye in their child.
Visual Evoked Potential (VEP) Exams
Visual Evoked Potential tests function of the visual pathway from the retina to the occipital cortex, the area at the back of the brain involved in receiving and interpreting visual signals. Three electrodes are placed on the head (similar to those of a heart monitor), and the child is shown alternating images on a computer screen. Brainwaves are gathered through the electrodes and results are produced on an electroencephalogram (EEG).
The test measures the time it takes for the visual stimulus to travel from the eye to the occipital cortex. As the nerve is compressed or damaged, electrical signals do not conduct properly, leading to a prolonged transmission time.
The test is most effective in detecting problems of the anterior optic nerve (the section from the optic disc where it exits the retina, to the chiasm, the part of the brain where the nerve from each eye crosses over). VEP is also valuable in assessing vision of children who cannot read eye charts.
Visual cortex cells are most sensitive to movement at the edge of the macula. VEP is ineffective in detecting problems of the anterior retina because we do not use this part of the retina to see.
VEP can be very valuable in detecting an optic pathway problem when cancer invades the macula. As retinoblastoma only arises from the macula in young babies, VEP is likely to be effective in early detection only for this age group. However, VEP is currently only available for children six months and older.
Retinoblastoma in children older than 6 months forms in the anterior retina. The child is likely to fail a VEP test only when the tumour has invaded the macula or other central parts of the eye, or when glaucoma or tumour itself compresses the optic nerve. Both glaucoma and optic nerve compression are indicators for emergent enucleation due to risk of cancer escaping the eye.
The older the child is when retinoblastoma first forms, the less likely the cancer is to be detected early by VEP.
Symptom Information in Expectant Mother Packs
Retinoblastoma advocacy charities in several countries have successfully campaigned to include information about early signs of retinoblastoma in Ministry of Health produced materials provided to expectant mothers. This simple information educates parents about the signs to look for and what to do if concerned, and becomes a resource they can present to doctors to back up their concerns and request for ophthalmology referral.
This approach is complicated in a country where resources for expectant mothers are developed by state or provincial health authorities, rather than by a national ministry. However, the process is no more complex than attempting to mandate regular eye exams, and with much greater impact as the information is put into the hands of the parent – the child’s key advocate.
Including information in the books is an excellent way of putting reliable information directly into the hands of mothers before their children are born, and is sustainable in the long term because the awareness process becomes funded by the state rather than by the charity or dedicated individual family.
Information card developed by Dr. Sandra Staffieri, Clinical and Research Orthoptist at the Centre for Eye Research Australia (CERA), and Retinoblastoma Care Co-ordinator at the Royal Children’s Hospital, Victoria.
Community Education
Providing information through leafleting to private homes, in commercial districts or at town fairs and other community events are all great ways to raise awareness among the general population. However, this approach is rarely cost effective as retinoblastoma is an uncommon cancer. Cost effectiveness measures cost of the campaign against the number of children diagnosed as a direct result of it.
Community education relies heavily on volunteers, and is sustainable only so long as people commit their time and energy to making it happen. Awareness that relies on this kind of education is unevenly distributed, putting children’s lives and sight at risk in under-served areas.
One also cannot monitor whether the distributed information is read, or the impact on early detection. So it is impossible to show what has been truly achieved for children, and clearly determine cost effectiveness of the campaign.
Media Coverage
The media has huge capacity to help raise awareness of retinoblastoma. Many excellent stories have been published around the world, promoting awareness of white pupil in a child’s photograph, and children’s lives have been saved as a result. Sadly, many families have frustrating stories of articles not including white pupil or squint information or example photographs, reporting facts incorrectly or sensationalizing their story such that the educational impact is lost.
Media coverage of retinoblastoma is hugely important, and is a vital adjunct to systematic early detection initiatives. But it should not be relied on as the only form of national awareness. In too many countries however, this is the only route families have to spread the retinoblastoma message widely.
Developing Effective Awareness Initiatives
All these approaches have a role to play in improving early diagnosis rates. Some are more sustainable and cost effective than others. Some will catch only certain presentations of retinoblastoma. Some require specific systems to exist before they can be implemented.
A truly effective national awareness program will most likely involve a mix of approaches, defined through careful planning and development. Here are some key questions the planning team will ask in developing a long-term sustainable awareness program:
- What is needed in this country / region?
- What existing systems can we build on?
- What is the potential to improve early diagnosis?
- What is the evidence for this approach?
- What is the reach of this approach (how many children)?
- What is the anticipated cost-effect of this approach?
- How can we measure impact?
- What is the potential for long term sustainability?
Awareness is One Part of the Retinoblastoma Triangle
Early diagnosis is only one part of the challenge. We must consider whether systems are in place to effectively refer and treat children, and support families, after early detection.
Early diagnosis becomes meaningless if a child is referred to a non-specialist hospital because an insurance provider dictates where they go. Or because the diagnosing doctor refers them to the esteemed ophthalmologist whom they trained with. Or because they simply don’t know where to send the family for expert care.
Early diagnosis is a hollow victory if treatment options are not based on clear evidence of value and risk to the whole child. Early diagnosis is a bitter success if resources are not available in the country to save at least one eye of a bilaterally affected child, when safe to do so.
Early diagnosis is squandered when eye-salvage therapy continues beyond the point of being safe. When removal of a dangerous eye is delayed and an otherwise curable child must fight for their life, or even lose their life.
Early diagnosis is a futile battle if a child is unable to access essential care due to lack of practical and emotional support for the family.
Early diagnosis is worthless if months or years of therapy without quality child life interventions harm the child’s natural development and emotional wellbeing. If the impacts of treatment trauma stay with them and their family and negatively influence their life path.
Awareness is the key starting point to give children the best opportunities for cure, but it is not a universal remedy to the challenges we face in bringing best care to children. Our global community has much work to do in building sustainable evidence based medical care and compassionate practical family support to ensure complete care for the entire family and effective cure for the child.
Thank you for joining us on this journey!
Join Us at One Rb World 2024 in Hawaii
Retinoblastoma awareness, early detection and care is a global challenge. There is no single solution, but many opportunities exist to improve early diagnosis, treatment and lifelong care in all regions of the world.
National and global collaboration between retinoblastoma specialists, researchers, parents, survivors, and other advocates can dramatically improve care and cure for each child with eye cancer, survivor and their family.
If you would like to join this global community sharing knowledge and experience, learning from one another, and exploring priority subjects together, we welcome you to the 7th One Rb World meeting, October 15-17 2024 in Honolulu, Hawaii. The meeting will be held just before the International Society of Paediatric Oncology World Congress which takes place 17-20 October, 2024 at the Honolulu Convention Centre.
One Rb World is community, conversation, and cooperation. An inclusive global collaboration for optimal lifelong care. Children are welcome too – One Rb World is proud to offer a full child life program for Rb patients, young survivors, siblings, and children of adult survivors!
Learn More About the Signs of Retinoblastoma
When ‘Something’ Looks the Same As ‘Nothing’ – learn more about strabismus, leukocoria and childhood eye cancer with this great article from Dr. Sandra Staffieri.







Leave a Reply
Want to join the discussion?Feel free to contribute!