Retinoblastoma Treatment and Vision – The Double-Edged Sword
Originally Published Monday August 3, 2020
When eye cancer is diagnosed early, it may be possible to save a child’s eye or even sight. But tumours and treatments themselves affect vision. Sandra Staffieri, orthoptist and Rb Care Co-ordinator at the Royal Children’s Hospital, Melbourne, reviews how different retinoblastoma therapies can impact the eye, and how parents can support their child.
When treating any child with retinoblastoma, there is no more important goal than to save their life.
With timely diagnosis and access to treatment, we may also be able to save the child’s eye or their sight. However, the process of saving eyes or vision can come at considerable cost – not just financially, but also the child’s emotional and long-term psychological wellbeing, as well as that of their parents, siblings, and extended family members. The cancer and its treatment, touches everyone.
The decision to pursue eye- or sight-saving treatment should be made with the child’s best interest at heart; can be a very difficult choice; and will be a very personal one for each family. Sometimes, there is no clear treatment pathway, and a variety of treatment options could be contemplated.
Together with their treating doctors, with careful consideration of the child’s individual situation, extent of the cancer and potential for saving their eye or sight, parents will make the treatment decision that is right for them. Not all families will choose the same treatment pathway for their child, even when the prognosis is the same. Respecting families’ individual decisions is critical.
Similarly, retinoblastoma may appear as “the same problem” between children from different families. But key factors that may be less well understood can in fact make the children’s situations very different, and thus the appropriate treatment options very different too.
For example, two children may both have cancer in one eye only. One child has a discrete, well-defined tumour at the very back of the eye (posterior pole). The other has disease that is more widely spread out (diffuse), and situated in the anterior chamber (front of the eye), very close to the structures that are common escape routes for the cancer (choroid, Schlemms canal – the eye’s fluid drainage system). The child with the discrete tumour may be more safely treated with intra-arterial chemotherapy, compared to the child with diffuse disease, who has a higher risk of cancer spreading beyond the eye.
Cause and Effect…
Tumours within the eye interfere with vision simply due to the area of the retina on which they have grown. Whilst we can try to control when we diagnose retinoblastoma, we cannot control where the tumours grow within the eye, or the negative effects of treatment to control the cancer.
Every treatment has its own inherent risks and benefits. The choice of treatment is determined by several factors such as the child’s age, location and size of tumours, and importantly, the potential for recovery or preservation of useful vision.
The eye is a very delicate organ in the body, and is sensitive to any treatments that may be used to control retinoblastoma. When used appropriately, no one treatment is better or worse than another in terms of their impact on vision. They each have their own problems and effect on vision or the eye – either immediately or many years after treatment.
Anatomy of the eye
Enucleation
Enucleation, surgical removal of the eye, was the first treatment to ever be recommended for retinoblastoma. Even though it was first used more than 170 years ago, enucleation continues to be the treatment of choice when disease in the eye is advanced and there is no or limited visual potential. It remains the most common treatment for advanced disease. If pathology after the surgery finds the cancer to be contained within the eye, enucleation is likely to be 100% curative.
Delaying enucleation in a child with advanced disease can risk the child’s life.
But how does enucleation, or losing one eye, affect vision and a child’s functioning? The reality is, in most children, if the cancer is so advanced within the eye that enucleation is considered, the child’s vision has likely already been affected. There is no guarantee their “vision” will change much after their surgery. Vision has already been lost. It can be very difficult to predict how much vision will be restored if eye-saving treatments are used, or how much the vision will be affected by the treatment itself, especially if the tumour has caused the retina to become detached.
When an eye is enucleated, three components of vision are affected:
- Central Vision
- Peripheral Vision
- Binocular Vision
Central Vision
When we look directly at an object, we use our central vision. The retinal cells we use for central vision are in the fovea or macula area. If the tumours cover this area, the vision will already be significantly affected. Removing the eye will not change the child’s central vision as they will continue to use the central vision they have in the other eye.
Peripheral Vision
Peripheral vision refers to the objects you see either side of another object you are looking directly at. When we measure the area of peripheral vision, it is referred to as the visual field. When we look with two healthy eyes, our visual fields overlap each other to a large degree.
The human visual field extends across 190 degrees in the horizontal plane.
A full visual field extends across 190 degrees. The visual field of each eye overlaps the blind spot that is created by the optic nerve exiting each eye. When you completely cover one eye, you will not be aware of this blind spot – the brain just “fills the information in”. An area of about 35 degrees on each side of the visual field can be seen with only the right or the left eye.
Following enucleation of one eye, the visual field that is lost will be the extreme 35 degrees, as shown in the diagram above. The eye that is removed will dictate which side of the visual field will be lost. It is not unusual for the child to bump into walls, people or objects on the side of their enucleated eye, although they usually adapt very quickly. Some children will learn to turn their head ever so slightly to move their visual field across to compensate for the 35 degrees lost, and sacrifice 17 degrees on each side.
Binocular Vision – Seeing In 3D
The sharpest 3D vision occurs when both eyes have relatively good and equal vision and are able to point in the same direction. 3D vision starts to develop soon after birth. This is why sometimes a baby’s eyes may look a little turned in soon after birth until the brain has learnt to use the two eyes together. A baby’s eye should be working together by 4-6 months of age.
Binocular vision – two eyes working together to see in 3D.
3D vision is the visual skill that is used to judge distances or the speed of objects that are travelling towards or away from us. Movies that are “3D” are a vastly exaggerated visual experience. If one eye has very poor vision, does not point in the same direction as the other eye or has been removed, the brain can readjust and will learn to judge distances and the speed of objects almost as well as if there were two eyes working normally. For these people however, the added visual experience of a 3D movie will be limited.
In an adult, presuming they had two healthy eyes that worked together correctly, and one eye had to be removed because of disease or injury, it would take about 3 months for the brain to adjust to the change in visual information. Children’s brains are much more adaptable than adults, and they take even less time to adjust.
After enucleation, many parents report their child’s visual behaviour is exactly the same or similar to what it was before the surgery. They are often surprised by this, but the reality is, their child had been adapting to the poor vision for a long time already – the central vision, the peripheral vision and the binocular vision.
Focal Therapies – Laser and Cryotherapy
Laser and cryotherapy are commonly used to directly treat retinoblastoma tumours. To be effective, the tumour must be of a certain size or volume. When tumours are detected early enough, these treatments can be applied directly, as a primary treatment. If the tumour is too large, it may first need to be shrunk with systemic or intra-arterial chemotherapy.
The cryotherapy or laser will also invariably damage some of the healthy surrounding retinal cells as well. With careful treatment, this can be minimised. Depending on the actual location on the retina, these tumours will determine the extent of the effect on the vision. Certainly, the tumour itself has already damaged any healthy retinal cells. If the tumour is in the area of the fovea and macula, then this treatment will affect the central vision. If the tumour is in the peripheral retina, then there will be a lesser impact on vision. Large areas of disease, even when treated with focal therapies will affect the peripheral vision.
Long-term, when there are extensive areas of laser or cryotherapy, the retina may become very damaged and detach. This will have a significant impact on vision, and successful repair may not be possible.
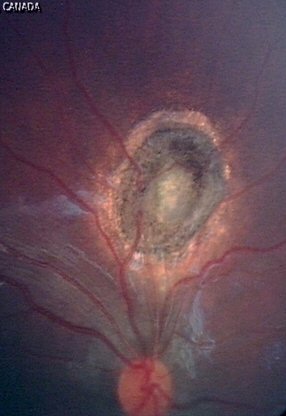
A very small tumour pre-treatment (yellow arrow); white burns immediately after laser; and 6 months later, regressed/controlled tumour with surrounding scar after 4 laser treatments.
Chemotherapy
Chemotherapy uses medications to destroy or damage the tumour cells. Unfortunately, it can also cause damage to healthy cells. The way the chemotherapy is actually delivered can increase or decrease these risks.
Intravenous Chemotherapy (IVC)
Intravenous chemotherapy has been successfully used to treat retinoblastoma for over 30 years. IVC affects rapidly dividing cells throughout the entire body, as well as cancer cells in the eye, and side effects occur when these healthy cells become damaged. In developed countries, children usually receive IVC through a central venous catheter (central line), which also has various benefits and risks, and requires special care.
Again, the location of the tumour itself on the retina will largely determine the effect on vision. If the tumour is in the area of central vision, the vision will still be affected, despite the treatment used to control it.
Intra-Arterial Chemotherapy (IAC)
Delivering a high dose of chemotherapy directly to the eye in theory makes a lot of sense as it reduces the effect of chemotherapy on healthy cells in the whole body, and this can work. IAC treatment and the procedure itself are not without risk, particularly when retinoblastoma is very advanced within the eye at diagnosis. But IAC has been shown to control tumours very well in some children.
Delivering such a high dose of a toxic chemical directly to the eye will also have a toxic effect on not only the tumour cells, but overall, to the healthy retinal cells. Research studies have shown that the electrical activity generated by healthy retinal cells diminishes by a small amount with each infusion, but may have some recovery.
Vision may also be affected as a direct result of the procedure itself. Although IAC is done by highly trained doctors, there are always risks. Because the chemotherapy is delivered directly into the main blood vessel that supplies the eye (ophthalmic artery), this blood vessel, or any or all of its branches could become blocked – even temporarily. Blockages could cause a loss of oxygen to the retinal cells (ischaemia), even healthy ones, and they die. Ischaemic retinal cells cease to function and so the vision served by that area of retina will be lost. If all the blood vessels are blocked, the whole eye becomes ischaemic and vision is completely lost.
There is still much to understand about the long-term effects of IAC, and we now need to wait and see what happens to children treated with IAC over time.
Intravitreal Chemotherapy (IVitC)
Intravitreal chemotherapy rose to prominence from 2012 when a safe technique was developed. Prior to this, puncturing the eyeball posed too high a risk of spilling active tumour cells outside of the eye, causing the cancer to spread. IVitC is used widely around the world to treat vitreous seeds, and is very effective in most cases. There are no reports of cancer spread outside the eye using this very careful technique. Many eyes are now being saved that would have previously been either enucleated or irradiated to treat the vitreous seeds.
As with IAC, injecting toxic chemicals directly into the eye will also have an effect in some way on the healthy retinal cells. The extent of vitreous disease, and which part of the vitreous the disease is in, will determine its effect on vision.
Time will tell what the long-term effects are of IVitC; there is still so much we do not know. But for now, it is a very useful treatment for vitreous disease that we didn’t have before, provided the main tumour from where the seeds are coming can be controlled.
Radiation
First used in the 1930s, radiation was the second treatment to be developed for retinoblastoma, other than enucleation. It worked very well and was used extensively for 50 years before the long-term effects and risks were better understood – particularly the risk of second primary cancers. For this reason, radiation is used in only the most extreme circumstances today.
Although radiation was an effective treatment for retinoblastoma, it can also damage the blood supply to the retina and cause ischaemia resulting in radiation retinopathy. This may occur soon after treatment or many, many years later, and can result in the patient losing previously good vision.
Radiation can indirectly affect vision by damaging the very sensitive corneal tissues. The cornea is the clear “front window” of the eye and is very sensitive to dryness. When the cornea becomes dry or damaged, this will significantly affect vision. Imagine a window that has become very scratched – you won’t be able to see through it.
Although plaque radiation does not have the same risk of developing second cancers in survivors with the RB1 mutation, it may also cause radiation retinopathy and have a significant effect on vision. Again, whilst all care is taken by the highly trained doctors using the plaques, there will always be some damage to healthy retinal cells and blood vessels in the surrounding areas.
A young girl enjoys a little play while waiting for treatment.
Retinoblastoma Treatments and Cataracts
We know that some treatments used to control retinoblastoma can also cause cataracts. This is particularly the case for radiation and intravitreal chemotherapy. A cataract is a clouding of the natural lens within the eye. As we age, cataracts are very common and can be surgically removed and replaced with an artificial lens. The results are largely excellent because the eye is otherwise healthy and developed normally.
Cataracts in children is a completely different problem because it can severely affect how the vision continues to develop. Timing of the surgery is also critical, as it would be very unwise to do cataract surgery in a child with active retinoblastoma disease. There is too high a risk for active tumour cells to spill out of the eye and spread. Any cataract surgery is delayed until there is complete long-term control of the cancer.
Retinoblastoma Treatments and Retinal Detachment
The retina is the light-sensitive tissue lining the eye that makes us see. It is made up of 10 layers of different cells and forms a ‘film’ much like the film in a traditional camera. Retinoblastoma can arise on top of or underneath this film. Tumours can push or pull the retina away from the choroid – the layer of blood vessels under the retina that supply it with oxygen and nutrients.
A retinal detachment may be present at the time of diagnosis if tumours have grown under the retinal film and pushed it up. As the tumour shrinks with treatment, the retina may reattach. Sometimes, retinal detachments occur after treatment to control the disease – including cryotherapy, laser therapy or IAC. As a tumour shrinks, it may pull on surrounding parts of the retina, causing it to detach. This is particularly common when a tumour shrinks very fast in response to treatment.
When the retina becomes detached, it is no longer able to function, resulting in severe vision loss.
Finding the Right Balance Between Treatment and Vision Loss
Treating retinoblastoma is a double-edged sword – determining the best treatment to provide maximum control of the cancer whilst minimising vision loss. All treatments will have some impact on vision, on top of the impact the tumour itself has had. These discussions are complex and individual to each child and family.
There is so much we do know, but there is also so much that we are yet to learn. The impact of enduring multiple, invasive treatments needs to be better understood, compared to a primary enucleation. There are still no controlled clinical trials comparing one treatment against another – all we can do right now is look back and evaluate the results of treatments in different children. This can be challenging when retinoblastoma is a rare disease, and most children are affected differently. We hope researchers working together from around the world will be happy to answer these questions.
Supporting Your Child with Vision Loss
It is clear that vision loss, in one way or another, goes hand in hand with a diagnosis of retinoblastoma. Depending on the degree of vision loss, there are some things you can do to help your child.
If Your Child Has Had An Enucleation
You can teach them to turn their head more fully to the side of their enucleation to make them safe, particularly when crossing roads. Most children will learn to do this themselves, but you can gently encourage them too.
When they attend kinder/nursery or school, you should mention to their teacher they have limited peripheral vision on the enucleated side. Your child should always be seated in the middle of the class or on the side of their enucleation so they don’t need to turn their head too far around to see what is happening at the front of the classroom. As your child gets older, they will become more confident about finding the best place in the classroom for them.
If Your Child Has A Vision Impairment
You should contact, or have your doctor refer you to, your local provider of low vision services. They will be able to give you strategies to stimulate your child’s vision and advise how best to provide a safe environment for your child. Engaging the services of low-vision experts can be confronting or even overwhelming, but they are best able to advise you to ensure your child can embrace and respond to their environment effectively, and support their needs as they change.
The following are starting points:
- The National Organization for Parents of Blind Children (USA)
- The American Printing House for the Blind
- Vision Serve Alliance (USA) can help you find a non-profit in your area
- Helen Keller National Centre (USA)
- Canadian National Institute for the Blind
- UK Royal National Institute for the Blind
- VICTA – for UK Children Teens and Young Adults with Sight-Loss
- Kenya Society for the Blind
- Vision Australia
- Royal Institute for Deaf and Blind Children (Australia)
- Blind Low Vision NZ
If you live in another country, you can reach out to any of these organizations to help you locate quality rehabilitation services near you.
Each of these organizations has networks of resources and signposts to other useful services. Some are locally or nationally government funded. Some are non-profit. Some are community-based, or paid for by health insurance, and some are national programs led by parents or blind and low vision people.
Children who live with sight-loss, cancer, and the stress it generates benefit from meeting and sharing their experiences. Here, a group of young retinoblastoma survivors and their siblings are co-creating a group board game, facilitated by a child life professional.
About the Author
Sandra Staffieri is the Retinoblastoma Care Co-ordinator at the Royal Children’s Hospital (RCH), Melbourne Australia. Working at the RCH and in private clinics, she has over 35 years’ experience in children’s eye health and disease.
As a Research Fellow and Clinical Orthoptist at the Centre for Eye Research Australia Sandra completed her PhD on delayed diagnosis of retinoblastoma. Her prime focus was to develop and evaluate an information pamphlet for new parents to raise awareness of the important signs of childhood eye disease – particularly strabismus and leukocoria – in the hope this could lead to earlier diagnosis of retinoblastoma.












Leave a Reply
Want to join the discussion?Feel free to contribute!